If you come from a typical South Asian-American family, then you’re intimately familiar with “sex”: how it’s everywhere and everyone’s doing it, but it’s never talked about and never acknowledged openly.
We hide “it” from our parents, we shy away from talk about it (or are written permission slips to escape it in school) and we tip-toe around it with our doctors. The result: before we know it, we’re facing reproductive health concerns that we don’t know how to begin to deal with.
[Read More: Parineeti Chopra Schools Male Journalist About Periods and Women’s Health]
If lucky, we start our sex-ed through covert gossip with friends, decent (though sometimes debauched) movies and books and common (but quickly deleted) internet searches. Many of us surely have stories to share that could have been less consequential had we had access to the biomedical knowledge and/or medical materials necessary to safely and effectively manage our sexual health.
While conducting a survey-based study and workshops on menstrual hygiene in India this past year, a 15-year-old schoolgirl from one of the topmost secondary schools in New Delhi—a large urban city and national capital—took me aside and asked:
Ma’am, is it okay for us to talk with boys? My mom doesn’t let me and says I’ll get pregnant.
That may be an extreme example of inadequate sex-ed, influenced in part by being raised in a sexually repressed and largely patriarchal developing nation.
But as immigrants, aren’t we simply an extension of that? Don’t we also bring with us similar myths and taboos in hopes of retaining original cultural values? What’s on our side, however, is that our youth are more capable of finding factual sources of sexual health information. This means that many know more than we did about STDs and pregnancy, they know things like when it comes to the symptoms of genital herpes men and women often don’t have any outward sign of infection, that you can’t catch HIV from a toilet seat etc. Yet still, there are some questions and issues that still need answers and increased awareness. Now that it’s 2016, possibly the year of a female POTUS, it’s high time that we take back the discussion about our own bodies.
Let’s start by debunking five myths prevalent in the South Asian-American community surrounding two controversial yet significant subjects: Contraception and the Human Papilloma Virus (HPV) vaccine.
1. South Asian youth don’t have premarital sex (or shouldn’t be), so parents and children don’t need to discuss these topics.
Initiating the conversation may be exceedingly awkward and possibly provoke a lifetime of grounding, but it’s essential that we have it. There are numerous sources of misinformation tainted by political leanings and unrealistic expectations of sex instilled by the advertising and film industries.
Given this, the conversation should start at home and with reputed healthcare professionals. Whether our betas and betis are bangin’ (insert eggplant emoji) before or after marriage, they should still have accurate information ahead of time to make responsible and safe decisions.
2. Contraception is only for those sexually active and to prevent pregnancy.
There are about 15 different types of contraceptives, such as condoms, diaphragms, oral pills, injections, implants, patches, IUDs (intrauterine devices), sterilization, and the emergency contraceptive pill. However, many women use contraception even when sexually inactive for reasons other than preventing pregnancy or protecting against sexually transmitted infections (STIs).
Varying in hormonal content, contraception can be used to regulate or control the timing of periods, lighten bleeding, reduce the pain from menstrual cramps (dysmenorrhea) and menstrual migraines, or help ease other symptoms of premenstrual syndrome (PMS). It can help clear acne and excessive body or facial hair growth (hirsutism). It can even help manage reproductive disorders like endometriosis and polycystic ovarian syndrome (PCOS), which can’t permanently be cured.
Aside from supporting safe sex, these additional benefits of contraception highlight how essential it is for health insurance companies to cover their high cost.
3. The HPV vaccine is only for women who are sexually active.
According to the CDC’s Division of Cancer Prevention and Control, the HPV vaccine should be administered to girls beginning at age 11 or 12. This is when the shot is most effective—even if they wait a while to become sexually active.
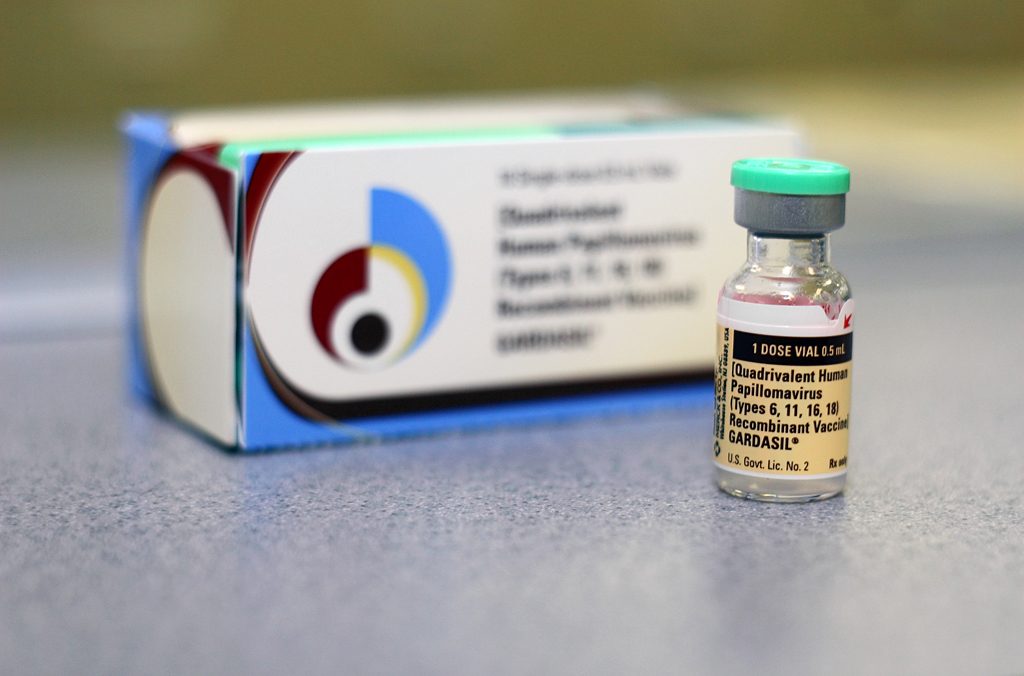
The HPV vaccine is the perfect excuse to initiate the sex talk, the pakshiyon and makhis (‘birds and the bees’) if you will. Two available HPV vaccines, Cervarix and Gardasil, are administered in a series of three shots to protect against the multiple strains of genital warts responsible for 70 percent of all cases of cervical cancer. And get this: the vaccine isn’t just for girls. It’s also recommended for males starting at age 11 to protect against genital warts, and oral, penis, and rectal cancers. The goal is to complete the series well before a child becomes sexually active.
About 15,000 HPV-associated cancers—including cervical, anal, vaginal, vulvar, and oropharyngeal—are seen in women each year in the US, yet may be prevented by the vaccine (CDC).
4. Contraception/the HPV vaccine cause long-term, life-threatening health consequences.
Imagine a TV commercial: a woman frolics about in a field of flowers and daydreams without a worry in the world. She’s a better woman because of these pills. Yet a monotone voice in the background fires off the following and scares you away: may cause weight gain, infertility, blood clots, migraines, stroke, and neurodegenerative disorders.
There are definitely mixed messages being sent, not to mention how a brown woman would never be cast—it’s not like we need these things, right? But what if we instead emphasize their health benefits?
Contraception: reduction in the risk of developing ovarian cysts; protection against ovarian, uterine, and colorectal cancers; increase fertility by preventing Pelvic Inflammatory Disease (PID); fewer miscarriages due to adequate spacing between pregnancies; bigger boobs (!!!); reduction in symptoms of premenstrual dysphoric disorder (PMDD); decrease in abortion rates.
HPV vaccine: prevents four common HPV types—16 and 18, two high-risk HPVs that cause about 70 percent of cervical and anal cancers, and 6 and 11, which cause 90 percent of genital warts; protects against new HPV strains.
5. Talking about and taking contraception/the HPV vaccine will encourage sexual activity, promiscuity, or riskier sexual behavior among South Asian youth.
This one is just ridiculous. If we wanted to do it, then we’re probably already doing it, which is the riskiest we can get anyway as unmarried South Asian youth. Might as well be healthy, safe, and empowered while we’re at it.




