One of our readers wanted the next women’s health column to focus on endometriosis and how it affects South Asian women. In an article published in September 2013 in MSNBC Health/Equality, South Asian women living with endometriosis spoke out about the lack of attention given to “invisible diseases” such as the one they live with everyday.
While we often speak about women’s health at Brown Girl Magazine, the point of this column is to discuss how women’s health issues are actualized in communities of color – largely focused on the South Asian community and those of the South Asian diaspora. Creating that awareness and outlet for women who struggle with life-altering health issues and giving their stories a voice – both through narrative and medical fact is a nuanced effect we hoped to achieve in this column. We always welcome suggestions for topics and for people to use Mahila Facts as a way to educate themselves, others, and to speak out/write about many of the health issues that South Asian women face in different sociopolitical contexts.
What is Endometriosis?
Endometriosis gets its name from the tissue that lines the uterus, called the endometrium. During the menstrual cycle, the endometrium grows and becomes thicker to allow for potential implantation of a fertilized egg. In the event of pregnancy, the endometrium continues to grow in size and the blood vessels within it fuse and eventually form the placenta. If fertilization does not occur, the endometrium breaks down and is shed from the body via the vagina during menstruation.
Your body goes through this cycle every month.
When the endometrium begins to grow outside of the uterus on other organs or body structures – such as the ovaries, fallopian tubes, pelvic cavity, outer area of the uterus, vagina, rectum, and/or bowel – the displaced tissue has no way of exiting the body. It becomes trapped and irritates the surrounding tissue and can lead to cysts and abnormal tissue growth.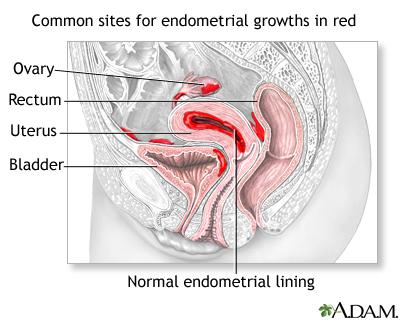
Who Gets It?
Any person who has menstrual periods can get endometriosis. However, it is more common for women in their 30s and 40s according to the U.S. Department of Health and Human Services Office of Women’s Health.
Symptoms
The primary symptom of endometriosis is pelvic pain, generally related to menstruation. During monthly periods, women cite menstrual pain that is “worse than usual cramping” and can often be debilitating to the point of skipping school, work, and/or daily activities. Often these issues go untreated without being properly diagnosed. Women also report that their pain increases over time.
One of the issues women with endometriosis face is that chronic and severe pelvic pain can be difficult to pinpoint to a specific cause. Endometriosis may be mistaken for many of the other conditions that also cause pelvic pain such as ovarian cysts (related to Polycystic Ovarian Syndrome), pelvic inflammatory disease (PID), or irritable bowel syndrome (IBS). According to the Mayo Clinic’s Endometriosis fact sheet, IBS can often accompany endometriosis further complicating the symptoms.
Common symptoms can include:
- Painful periods:
- Painful cramping during menstruation that is bad enough to keep you from doing daily activities
- Pain can begin several days before your period and last several days afterwards
- Chronic lower back, intestinal, and/or pelvic pain
- Pain during or after sexual intercourse
- During menstruation, pain during urination and bowel movements.
- Spotting or bleeding between menstrual periods and heavy periods (excessive bleeding during menstruation)
- Infertility or not being able to get pregnant because the endometrial tissue can cover and grow into your ovaries and block the fallopian tubes making ovulation and fertilization difficult.
- Fatigue, diarrhea, constipation, bloating, and/or nausea, especially during menstrual periods (can be associated with symptoms of IBS as well).
How is Endometriosis Diagnosed?
You may first go see your primary care doctor or OB/GYN. Often it is difficult to remember all of your symptoms, the frequency at which you experience them, and/or family history. We also often feel uncomfortable discussing certain aspects of our bodies, sexual lives, and “embarrassing symptoms.”
Therefore, it’s important to prepare yourself in advance with 1) the questions you want to ask of the doctor; 2) sharing details that may seem uncomfortable or embarrassing. If you have already been seen by another doctor for the same symptoms or if you have previous test results or scans on hand, bring them with you.
As a college student and now as a 20-something woman living on my own, I like to make sure I am in charge of my medical history so that I can be as informed and aware of my own body. I bring a small notepad or use the notes application in my iPhone to both write down questions I have for the doctor and make notes during all of my doctor’s visits. Coming armed with both an awareness of what is happening as well as with basic questions can help the visit go smoothly and also give you a sense of empowerment in having some stake in your own care. While I cannot understand the experiences of women who live with endometriosis, I believe this general practice can be helpful both practically and mentally.
Before your visit consider doing the following:
- Make a list of symptoms (even the ones that seem like “they aren’t that big of a deal.”) You may not see how many of the symptomsare related, but it can help the doctor better pinpoint your diagnosis.
- Know if there are things that make your symptoms better or worse
- Try to write down frequency of symptoms and severity
- Write down all of the medications you have taken recently or are currently taking. It’s good practice to also list the vitamins and other supplements you take.
- Prepare a list of questions you want to ask the doctor based on what is important to you:
- How is endometriosis diagnosed?
- What medications can I take? What are the side-effects of those medications?
- Can I get pregnant? What are the precautious I have to take?
- Is surgery right for me?
- What are the pros and cons of medications vs. surgery?
- Are their alternative treatments such as lifestyle changes or self-care I can try?
In diagnosing endometriosis, you doctor will conduct one or more of the following:
- Physical pelvic exam: The doctor will conduct this exam to feel for large cysts or scars in the uterine area. Smaller cysts and regions are often missed through a physical exam.
- Vaginal, Pelvic, and/or Abdominal Ultrasound: The doctor can use this imaging test look at various reproductive organs and look for the signs of cysts or abnormal tissue growth.
- Laparoscopy: This is a minor surgery that allows the doctor to look inside your abdomen for growth created by the endometriosis. The doctor may be able to diagnose you based on the appearance of tissue growth. Other times, the doctor will take a small tissues sample and use a microscope to make the diagnosis.
How is Endometriosis Treated?
Endometriosis has no cure, but several treatments can help manage the condition. The treatment you ultimately choose to receive will be based on a number of factors including your symptoms, age, and pregnancy plans.
- Pain medication. Over the counter medications such as Advil or Motrin can be used to alleviate mild pain symptoms. Doctors can also prescribe stronger pain relievers if the over the counter medications do not help.
- Hormone treatment. Often hormonetreatmentcan be used for women who do not plan to get pregnant. Some of the different hormone therapies include:
- Birth control pills: These can help decrease the flow during menstruation and the overgrowth of endometrial tissue.
- GnRH agonists: GnRH stands for gonadotropin releasing hormone and it is a key player in the menstrual cycle. These agonists reduce estrogen levels and subsequently stop the menstrual cycle. This drugs can cause similar side effects to the ones experienced during menopause such as a hot flashes, bone thinning ,and vaginal dryness.
- Progestins: The hormone progestin can shrink spots of endometrisis on the tissue. Progestin will also stop menstruation. Depo-Provera is a more common name for progestin that is taken via injection. Side effects of progestin can include weight gain, depressed mood, and decreased bone growth.
- Surgery: There are both minor and complex surgeries that can help with severe endometriosis and infertility issues.
- Laparoscopy: This surgery can be used to diagnose and treat endometriosis as discussed above.
- Laparotomy: This is more of a major abdominal surgery and it involves a much larger cut in the abdomen. Doctors can then remove endometriosis growth in the pelvis or abdomen.
- Hysterectomy: In this surgery, the doctor removes the entire uterus. Often the ovaries are removed as well so that the endometriosis cannot return and this means a woman cannot get pregnant afterwards. The hyerectromy is a last resort and only recommended for women over a certain age.
Self-Care and Emotional Health with Endometriosis
Dealing with any life-altering condition can lead to emotional and mental struggle. Ask your doctor for alternative methods and home remedies that can help with managing your endometriosis in addition to your preferred treatment plan.
Often a diet that consists of low refined carbohydrates and limited in caffeine, red meat, and processed foods can help you feel better about your health and body. Communicating with your partner about how endometriosis affects sex and experimenting can help avoid situations that create severe pain.
Many South Asian women may find dealing with the social and cultural manifestations of endometriosis to be difficult in their communities and families where reproductive and sexual health issues are not openly discussed. However, as the MSNBC article points out:
“If we want a world where all women, including women of color, are empowered to make their own healthcare decisions…we must challenge the social, economic and cultural barriers to care—for all diseases.”
Demystifying the science behind a condition, arming yourself with information and a practical plan of action, and sharing experiences are a couple of ways we can challenge and eventually break those barriers – both internal and external.
For more information and links to support groups on Endometriosis:
Endometriosis.org: The Global Forum
The Endometriosis Association www.EndometriosisAssn.org or www.KillerCramps.org
*Medical Disclaimer: We are not medical doctors and therefore cannot give medical advice or diagnose any condition. The information in this article is for educational purposes and to raise awareness, especially in the South Asian community where these issues are often not discussed. Please consult a physician.

Vaidehi Mujumdar is an aspiring physician, writer, and researcher based in Washington DC. She’s a contributing writer for India.com’s US Edition. Her work has been published in The Guardian, The Feminist Wire, Media Diversified, and others. See more of Vaidehi’s work on her website.




